Volume 10, Issue 1 (1-2024)
Journal of Research in Applied and Basic Medical Sciences 2024, 10(1): 88-93 |
Back to browse issues page
Ethics code: HIMS/IRC/21/22
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
B E C, KP A, Kumar M. Spectrum of neural tube defect in fetal autopsies. Journal of Research in Applied and Basic Medical Sciences 2024; 10 (1) :88-93
URL: http://ijrabms.umsu.ac.ir/article-1-276-en.html
URL: http://ijrabms.umsu.ac.ir/article-1-276-en.html
Senior Resident, Department of Pathology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India , Chaitrabe93@gmail.com
Full-Text [PDF 295 kb]
(867 Downloads)
| Abstract (HTML) (1897 Views)
Full-Text: (713 Views)
Introduction
WHO defines congenital anomalies as structural or functional anomalies that occur during intrauterine life. According to the March of Dimes (MOD) global report on birth defects, 7.9 million births (6% of total births) occur annually worldwide with serious birth defects, and 94% of these births occur in middle and low-income countries (1). According to the March of Dimes report in 2006, the prevalence of congenital anomalies in India is 6-7%, which translates to around 1.7 million birth defects annually. The common birth defects include congenital heart disease (8-10 per 1000 live births), congenital deafness (5.6-10 per 1000 live births), and neural tube defects (4-11.4 per 1000 live births)(1).
Neural tube defects (NTD) are the congenital malformations of the central nervous system. NTDs result from the failure of closure of the neural tube between the 3rd - 4th week of intrauterine development. Worldwide, NTDs affect 323,904 infants and cause 88,000 deaths every year, in addition to leaving 8.6 million people with disabilities. They are the cause behind 29% of neonatal deaths in low-income countries. The prevalence of these malformations ranges from 0.5 to 2 per 1000 births in countries without folic acid supplementation(2). The prevalence of NTDs in India has been reported to vary from 0.5 to 11 per 1000 births(3).
Classically, NTDs are divided into two main groups: defects affecting brain structures (anencephaly and encephalocele) and structures of the spinal cord (meningocele, myelomeningocele, and other forms of spina bifida). Anencephaly results from the failure of neurulation in the cephalic region, and is characterized by the absence of a large part of the brain and overlying skull. Exencephaly (the embryonic precursor to anencephaly) occurs when closure fails in the anterior neural plate or brain. Encephalocele occurs when the cranial vault fails to form properly around the closed neural tube and the brain and meninges protrude through an opening in the skull. Spina bifida is a failure of neural tube closure in the posterior region of the embryo and is classified into a number of forms including: meningocele where the meninges protrude from an opening in the vertebrae; myelomeningocele where the meninges and spinal cord protrude from an opening in the vertebrae, and spina bifida occulta where the dorsal part of the vertebrae does not form but neither the meninges nor the spinal cord protrude. Craniorachischisis is the most severe NTD, resulting from the failure of neural tube closure along the entire neural plate. Anencephaly and craniorachischisis are fatal, resulting in prenatal death of the fetus or demise of the newborn shortly after birth (4).
The WHO subclassifies CNS anomalies under the group, “Congenital malformations of the nervous system” (Q00-Q07) ICD 10 Code as Q00 for Anencephaly and similar malformations, Q01 for Encephalocele, Q02 for Microcephaly, Q03 for Congenital hydrocephalus, Q04 for Other congenital malformations of brain, Q05 for Spina bifida, Q06 for Other malformations of spinal cord, Q07 for Other malformations of nervous system(1).
The exact causes of NTDs are not known. Many different factors, including genetics, nutrition like folic acid and environmental factors, are known to play a role. Geography, race, maternal obesity, antiepileptic drug use, pesticide exposure, smoking, indoor air pollution from predominantly biomass heating, X-ray radiation exposure, family history, and previous history of stillbirth have been reported to contribute to the development of NTDs (5).
In recent studies, chromosomal anomalies such as trisomy 13, trisomy 18 and triploidy represent less than 10% of all NTDs cases, while non-syndromic isolated cases represent the vast majority of NTDs, exhibiting a sporadic pattern of occurrence. In terms of genetic predisposition, women show a recurrence risk rate of 3% after conceiving a NTD embryo and 10% after conceiving a second NTD embryo. Female gender predisposition has been reported for some types of NTDs, possibly due to a sex-related genetic or epigenetic effect. Despite the decades long attempts to elucidate genetic factors causative of NTDs in humans, no conclusive evidence has been identified(20).
Although prenatal sonography has been developed in recent years, the definitive diagnosis of fatal fetal malformations is best made by fetal autopsy. An autopsy of congenital malformations not only confirms, but also provides additional information and is useful in advising parents about the risks and prevention of similar malformations in future pregnancies.
Aims: To study the spectrum of neural tube defect in foetal autopsies
Materials & Methods
This retrospective study was conducted in the Department of Pathology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India. The cases originated from still birth, spontaneous and therapeutic abortion. Ninety-seven fetal autopsies were performed between July 2010 and June 2020, out of which 39 cases had CNS malformations. Thirty-six cases with neural tube defects were included in this study. All the essential clinical data such as gestational age, gender, birth weight, mode of delivery, maternal age, gravidity of mother, history of consanguinity and previous abortions, maternal comorbidities, and intake of folic acid supplements were retrieved from the autopsy forms and case files. In every case, the location and morphology of the NTD and associated morphological anomalies were noted. The statistical analysis was performed using frequency and percentage with SPSS version 24.
Results
.png)
A total of 36 cases of fetal autopsies with NTD were analysed. The majority of the fetuses, 22 (61.1%), with NTD were aborted at the gestational age of 20-24 weeks. Out of these, 27 (75%) of fetuses were females. The majority of the fetuses, 28 (77.78%), had a birth weight less than 1000 grams, while 6 (16.67%) had a birth weight of 1000-2000 grams and 2 had a birth weight of 3000 grams. The maternal age ranged from 18-35 years. The majority of congenital anomalies were found in the maternal age group between 20-25 years, constituting 19 (52.78%). Out of the mothers, 20 (55.5%) were primigravida. 6 (16.67%) mothers had a history of consanguinity. Additionally, 7 (19.44%) mothers had a history of prior abortion. 11 (30.56%) mothers had morbidity in the form of hypertension and diabetes. The history of intake of Folic acid as a supplement was not available in 23 (63.89%) cases. Among 39 cases with CNS malformations, 36 cases had neural tube defects. The majority of the cases were diagnosed with spina bifida (27.78%), followed by anencephaly (25%). The distribution of various neural tube defects is shown in the (chart 1).
Fig. 1. Yearly distribution of NTD among 10 years
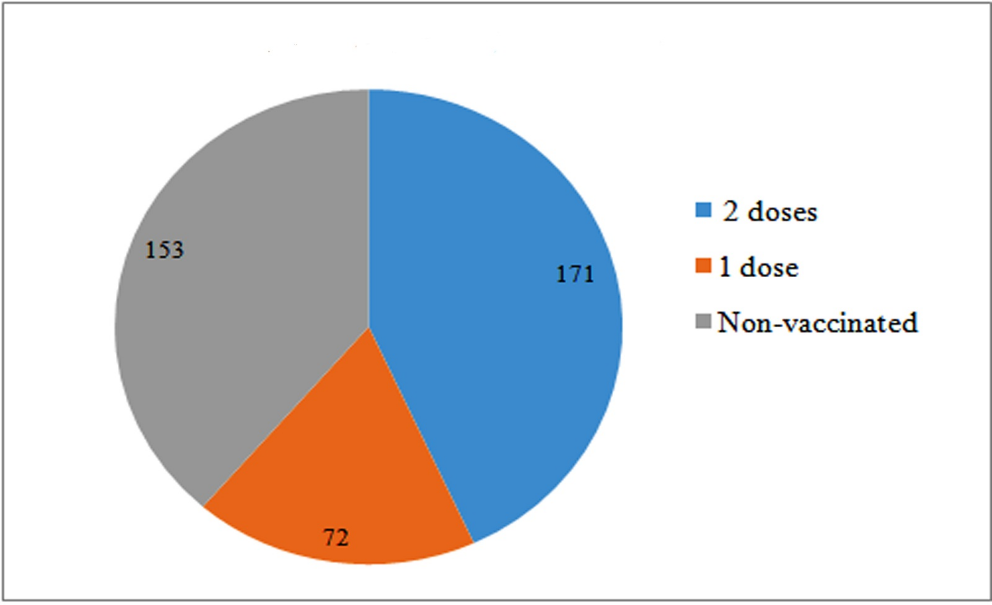
Chart 1. Distribution of various cases of NTDDiscussion
Neural tube defects (NTDs) are a group of severe congenital malformations of the central nervous system resulting from failure of neural tube closure during early embryonic life. Neural tube formation occurs before day 28 of human embryonic development. The process begins with the laying down of the neural plate, which then curves upward and fuses to form the neural tube, a process known as primary neurogenesis. Secondary neurogenesis, also called canalization, involves the formation of a continuous lumen of the neural tube. Neural tube fusion is now thought to involve five closure sites that may represent weak points in the developing spine.
NTD is generally considered a multifactorial cause, involving genetic and environmental factors. The factors identified as potential risk factors can be divided into fetal and maternal factors. Fetal factors include environmental damage to the fetus in early pregnancy. Maternal factors include advanced age, history of miscarriage, and family history of twins or NTDs. In addition, dietary factors such as folic acid, gestational diabetes, medications, and genetics are associated with risk factors.
Various theories of Neural Tube Closure were given to describe the neural tube defects in animal models and in humans. Van Allen et al. (1993) compared the multisite model vs. the traditional single-site model of neural tube closure for the best explanation for NTDs in humans. With the multi-site neural tube closure model, the majority of NTDs can be explained by failure of fusion of one of the closures or their contiguous neuropores. In NTDs, the first defect is in the notochord development resulting in failure of the neural folds to fuse in the midline and to make a normal neural tube. The next defect is the failure of the mesoderm to develop. Failure of mutual induction of all three germ layers in temporally related sequence can lead to various types of NTDs. Various genetic factors were studied in animal models regulating the neurulation process. Noggin, Chordin, and Folistatin, secreted by notochord and primitive node, lead to the inhibition of BMP4 which is required for the conversion of ectoderm to neuroectoderm and to dorsalize the mesoderm to paraxial mesoderm. Various other genes like WNT, FGF (Fibroblast Growth Factor), and SHH (Sonic Hedge Hog) were also described as controlling the different phases of neurulation.
In the present study, the gestational age of 20-24 weeks was the most common age of fetus with NTD, which is in concordance with findings of study by Rajesh H Chandan et al… Female (75%) predominance was seen in the present study, similar to the study done by Rajesh H Chandan et al., and Struksnæs C et al… Most fetuses had birth weight of less than 1000 gms (77.78%) in the present study, similar to study by Rajesh H Chandan et al., and Kale-Jain PP et al… In the present study, the most common maternal age was between 20 -25 years, which is in concordance with study by Rajesh H Chandan et al., and Struksnæs C et al… The present study reported primigravida mothers had more incidence (55.5%) of congenital anomalies, similar to study done by Rajesh H Chandan et al. and Sivashankara et al…
Several studies have reported the role of consanguinity in the occurrence of congenital malformations. These malformations are twice as likely to occur in the case of first cousins. In Forci et al., study, consanguinity was notified in different types of NTDs with an estimated rate of 34% and even 80% in first-degree cases. In the present study, consanguinity is seen in 6 cases. Seven cases had a history of abortion (19.4%) in the present study, similar to findings by Rajesh H Chandan et al., and Kale-Jain PP et al… Eleven (30.56%) mothers had morbidity in the form of hypertension and diabetes. In the study done by Vinutha et al., Maternal diabetes, hypertension, and hypothyroidism showed a positive correlation with congenital anomalies with a significant association between maternal hypothyroidism and CNS anomaly in the stillborn fetus.
The history of intake of Folic acid as a supplement was not available in the 23 cases (63.89%). The major thrust of primary prevention of NTDs has been on nutritional supplementation with folic acid apart from controlling the maternal diseases like diabetes and avoiding medications. Role of 0.4 mg of periconceptional folic acid leading to reduction in NTDs was demonstrated by MRC, and also by Kulkarni et al. in India. Currently, there is no national program for primary prevention of NTD in India. National anemia prevention program provides 0.5 mg of folic acid along with 100 mg of elemental iron from the third month of pregnancy. The recent National Family Health Survey (NFHS-3) revealed that about 56% of pregnant women sought antenatal care after 16 weeks of gestation. Thus, only a small percentage of women receive Periconceptional folic acid supplementation. Fifty-four countries, including India, are practicing fortification of flour with folic acid. There was a decline in the incidence of anencephaly after fortification in the USA, South Africa, Canada, and Singapore. Fortification of flour in India is not uniform; it varies from state to state with the highest percentage in Gujarat. The benefit of fortification of flour still needs to be established in India. Fortification of folic acid is a two-edge sword as it may cause prevention of anencephaly but is a risk factor for colorectal cancer and neuro-cognitive decline.
In the present study, spina bifida was more common (27.78%) followed by anencephaly (25%), which is similar to the study done by Garg.S.et al., Kant.et al., Cherian et al., Zaganjor et al., whereas contrast to studies done by Kulakrni et al, Mini et al, Bhide et al., where incidence of anencephaly was more as compared to other NTDs.
Conclusion
Congenital disorders are great public health issues in developing countries. Neurological anomalies are among the most common congenital defects which are also fatal. The multidisciplinary approaches to fetal malformations have ever-increasing importance in prenatal medicine. Fetal autopsy has a vital role in diagnosis of congenital malformations and detecting cause of death and can give clues to clinicians to estimate risk of recurrence and genetic counseling. Primary prevention through mandatory folic acid supplementation seems to be the more rational solution in line with global progress. Initiation of a public health program to prevent NTD cases by fortifying staple foods with folic acid should be urgently addressed. A congenital anomaly surveillance system establishment should also be considered to monitor the progress.
Acknowledgments
None.
Conflict of interest:
The authors declare that they have no conflicts of interest.
Funding/support:
None.
Data Availability
The raw data supporting the conclusions of this article are available from the authors upon reasonable request.
Ethical statement (Code):
This research was conducted in accordance with ethical principles (HIMS/IRC/21/22).
Author contributions:
- Article idea and writing: Dr. Chaitra B.E.
- Data collection: Dr. Mohit Kumar
- Statistical analysis: Dr. Athira K.P.
WHO defines congenital anomalies as structural or functional anomalies that occur during intrauterine life. According to the March of Dimes (MOD) global report on birth defects, 7.9 million births (6% of total births) occur annually worldwide with serious birth defects, and 94% of these births occur in middle and low-income countries (1). According to the March of Dimes report in 2006, the prevalence of congenital anomalies in India is 6-7%, which translates to around 1.7 million birth defects annually. The common birth defects include congenital heart disease (8-10 per 1000 live births), congenital deafness (5.6-10 per 1000 live births), and neural tube defects (4-11.4 per 1000 live births)(1).
Neural tube defects (NTD) are the congenital malformations of the central nervous system. NTDs result from the failure of closure of the neural tube between the 3rd - 4th week of intrauterine development. Worldwide, NTDs affect 323,904 infants and cause 88,000 deaths every year, in addition to leaving 8.6 million people with disabilities. They are the cause behind 29% of neonatal deaths in low-income countries. The prevalence of these malformations ranges from 0.5 to 2 per 1000 births in countries without folic acid supplementation(2). The prevalence of NTDs in India has been reported to vary from 0.5 to 11 per 1000 births(3).
Classically, NTDs are divided into two main groups: defects affecting brain structures (anencephaly and encephalocele) and structures of the spinal cord (meningocele, myelomeningocele, and other forms of spina bifida). Anencephaly results from the failure of neurulation in the cephalic region, and is characterized by the absence of a large part of the brain and overlying skull. Exencephaly (the embryonic precursor to anencephaly) occurs when closure fails in the anterior neural plate or brain. Encephalocele occurs when the cranial vault fails to form properly around the closed neural tube and the brain and meninges protrude through an opening in the skull. Spina bifida is a failure of neural tube closure in the posterior region of the embryo and is classified into a number of forms including: meningocele where the meninges protrude from an opening in the vertebrae; myelomeningocele where the meninges and spinal cord protrude from an opening in the vertebrae, and spina bifida occulta where the dorsal part of the vertebrae does not form but neither the meninges nor the spinal cord protrude. Craniorachischisis is the most severe NTD, resulting from the failure of neural tube closure along the entire neural plate. Anencephaly and craniorachischisis are fatal, resulting in prenatal death of the fetus or demise of the newborn shortly after birth (4).
The WHO subclassifies CNS anomalies under the group, “Congenital malformations of the nervous system” (Q00-Q07) ICD 10 Code as Q00 for Anencephaly and similar malformations, Q01 for Encephalocele, Q02 for Microcephaly, Q03 for Congenital hydrocephalus, Q04 for Other congenital malformations of brain, Q05 for Spina bifida, Q06 for Other malformations of spinal cord, Q07 for Other malformations of nervous system(1).
The exact causes of NTDs are not known. Many different factors, including genetics, nutrition like folic acid and environmental factors, are known to play a role. Geography, race, maternal obesity, antiepileptic drug use, pesticide exposure, smoking, indoor air pollution from predominantly biomass heating, X-ray radiation exposure, family history, and previous history of stillbirth have been reported to contribute to the development of NTDs (5).
In recent studies, chromosomal anomalies such as trisomy 13, trisomy 18 and triploidy represent less than 10% of all NTDs cases, while non-syndromic isolated cases represent the vast majority of NTDs, exhibiting a sporadic pattern of occurrence. In terms of genetic predisposition, women show a recurrence risk rate of 3% after conceiving a NTD embryo and 10% after conceiving a second NTD embryo. Female gender predisposition has been reported for some types of NTDs, possibly due to a sex-related genetic or epigenetic effect. Despite the decades long attempts to elucidate genetic factors causative of NTDs in humans, no conclusive evidence has been identified(20).
Although prenatal sonography has been developed in recent years, the definitive diagnosis of fatal fetal malformations is best made by fetal autopsy. An autopsy of congenital malformations not only confirms, but also provides additional information and is useful in advising parents about the risks and prevention of similar malformations in future pregnancies.
Aims: To study the spectrum of neural tube defect in foetal autopsies
Materials & Methods
This retrospective study was conducted in the Department of Pathology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India. The cases originated from still birth, spontaneous and therapeutic abortion. Ninety-seven fetal autopsies were performed between July 2010 and June 2020, out of which 39 cases had CNS malformations. Thirty-six cases with neural tube defects were included in this study. All the essential clinical data such as gestational age, gender, birth weight, mode of delivery, maternal age, gravidity of mother, history of consanguinity and previous abortions, maternal comorbidities, and intake of folic acid supplements were retrieved from the autopsy forms and case files. In every case, the location and morphology of the NTD and associated morphological anomalies were noted. The statistical analysis was performed using frequency and percentage with SPSS version 24.
Results
.png)
A total of 36 cases of fetal autopsies with NTD were analysed. The majority of the fetuses, 22 (61.1%), with NTD were aborted at the gestational age of 20-24 weeks. Out of these, 27 (75%) of fetuses were females. The majority of the fetuses, 28 (77.78%), had a birth weight less than 1000 grams, while 6 (16.67%) had a birth weight of 1000-2000 grams and 2 had a birth weight of 3000 grams. The maternal age ranged from 18-35 years. The majority of congenital anomalies were found in the maternal age group between 20-25 years, constituting 19 (52.78%). Out of the mothers, 20 (55.5%) were primigravida. 6 (16.67%) mothers had a history of consanguinity. Additionally, 7 (19.44%) mothers had a history of prior abortion. 11 (30.56%) mothers had morbidity in the form of hypertension and diabetes. The history of intake of Folic acid as a supplement was not available in 23 (63.89%) cases. Among 39 cases with CNS malformations, 36 cases had neural tube defects. The majority of the cases were diagnosed with spina bifida (27.78%), followed by anencephaly (25%). The distribution of various neural tube defects is shown in the (chart 1).
Fig. 1. Yearly distribution of NTD among 10 years
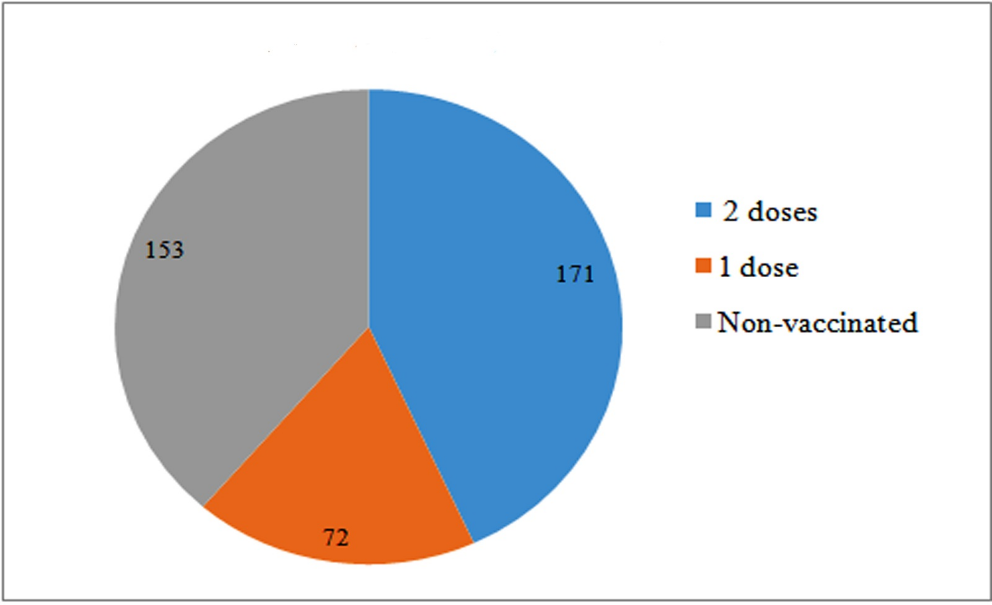
Chart 1. Distribution of various cases of NTDDiscussion
Neural tube defects (NTDs) are a group of severe congenital malformations of the central nervous system resulting from failure of neural tube closure during early embryonic life. Neural tube formation occurs before day 28 of human embryonic development. The process begins with the laying down of the neural plate, which then curves upward and fuses to form the neural tube, a process known as primary neurogenesis. Secondary neurogenesis, also called canalization, involves the formation of a continuous lumen of the neural tube. Neural tube fusion is now thought to involve five closure sites that may represent weak points in the developing spine.
NTD is generally considered a multifactorial cause, involving genetic and environmental factors. The factors identified as potential risk factors can be divided into fetal and maternal factors. Fetal factors include environmental damage to the fetus in early pregnancy. Maternal factors include advanced age, history of miscarriage, and family history of twins or NTDs. In addition, dietary factors such as folic acid, gestational diabetes, medications, and genetics are associated with risk factors.
Various theories of Neural Tube Closure were given to describe the neural tube defects in animal models and in humans. Van Allen et al. (1993) compared the multisite model vs. the traditional single-site model of neural tube closure for the best explanation for NTDs in humans. With the multi-site neural tube closure model, the majority of NTDs can be explained by failure of fusion of one of the closures or their contiguous neuropores. In NTDs, the first defect is in the notochord development resulting in failure of the neural folds to fuse in the midline and to make a normal neural tube. The next defect is the failure of the mesoderm to develop. Failure of mutual induction of all three germ layers in temporally related sequence can lead to various types of NTDs. Various genetic factors were studied in animal models regulating the neurulation process. Noggin, Chordin, and Folistatin, secreted by notochord and primitive node, lead to the inhibition of BMP4 which is required for the conversion of ectoderm to neuroectoderm and to dorsalize the mesoderm to paraxial mesoderm. Various other genes like WNT, FGF (Fibroblast Growth Factor), and SHH (Sonic Hedge Hog) were also described as controlling the different phases of neurulation.
In the present study, the gestational age of 20-24 weeks was the most common age of fetus with NTD, which is in concordance with findings of study by Rajesh H Chandan et al… Female (75%) predominance was seen in the present study, similar to the study done by Rajesh H Chandan et al., and Struksnæs C et al… Most fetuses had birth weight of less than 1000 gms (77.78%) in the present study, similar to study by Rajesh H Chandan et al., and Kale-Jain PP et al… In the present study, the most common maternal age was between 20 -25 years, which is in concordance with study by Rajesh H Chandan et al., and Struksnæs C et al… The present study reported primigravida mothers had more incidence (55.5%) of congenital anomalies, similar to study done by Rajesh H Chandan et al. and Sivashankara et al…
Several studies have reported the role of consanguinity in the occurrence of congenital malformations. These malformations are twice as likely to occur in the case of first cousins. In Forci et al., study, consanguinity was notified in different types of NTDs with an estimated rate of 34% and even 80% in first-degree cases. In the present study, consanguinity is seen in 6 cases. Seven cases had a history of abortion (19.4%) in the present study, similar to findings by Rajesh H Chandan et al., and Kale-Jain PP et al… Eleven (30.56%) mothers had morbidity in the form of hypertension and diabetes. In the study done by Vinutha et al., Maternal diabetes, hypertension, and hypothyroidism showed a positive correlation with congenital anomalies with a significant association between maternal hypothyroidism and CNS anomaly in the stillborn fetus.
The history of intake of Folic acid as a supplement was not available in the 23 cases (63.89%). The major thrust of primary prevention of NTDs has been on nutritional supplementation with folic acid apart from controlling the maternal diseases like diabetes and avoiding medications. Role of 0.4 mg of periconceptional folic acid leading to reduction in NTDs was demonstrated by MRC, and also by Kulkarni et al. in India. Currently, there is no national program for primary prevention of NTD in India. National anemia prevention program provides 0.5 mg of folic acid along with 100 mg of elemental iron from the third month of pregnancy. The recent National Family Health Survey (NFHS-3) revealed that about 56% of pregnant women sought antenatal care after 16 weeks of gestation. Thus, only a small percentage of women receive Periconceptional folic acid supplementation. Fifty-four countries, including India, are practicing fortification of flour with folic acid. There was a decline in the incidence of anencephaly after fortification in the USA, South Africa, Canada, and Singapore. Fortification of flour in India is not uniform; it varies from state to state with the highest percentage in Gujarat. The benefit of fortification of flour still needs to be established in India. Fortification of folic acid is a two-edge sword as it may cause prevention of anencephaly but is a risk factor for colorectal cancer and neuro-cognitive decline.
In the present study, spina bifida was more common (27.78%) followed by anencephaly (25%), which is similar to the study done by Garg.S.et al., Kant.et al., Cherian et al., Zaganjor et al., whereas contrast to studies done by Kulakrni et al, Mini et al, Bhide et al., where incidence of anencephaly was more as compared to other NTDs.
Conclusion
Congenital disorders are great public health issues in developing countries. Neurological anomalies are among the most common congenital defects which are also fatal. The multidisciplinary approaches to fetal malformations have ever-increasing importance in prenatal medicine. Fetal autopsy has a vital role in diagnosis of congenital malformations and detecting cause of death and can give clues to clinicians to estimate risk of recurrence and genetic counseling. Primary prevention through mandatory folic acid supplementation seems to be the more rational solution in line with global progress. Initiation of a public health program to prevent NTD cases by fortifying staple foods with folic acid should be urgently addressed. A congenital anomaly surveillance system establishment should also be considered to monitor the progress.
Acknowledgments
None.
Conflict of interest:
The authors declare that they have no conflicts of interest.
Funding/support:
None.
Data Availability
The raw data supporting the conclusions of this article are available from the authors upon reasonable request.
Ethical statement (Code):
This research was conducted in accordance with ethical principles (HIMS/IRC/21/22).
Author contributions:
- Article idea and writing: Dr. Chaitra B.E.
- Data collection: Dr. Mohit Kumar
- Statistical analysis: Dr. Athira K.P.
Type of Study: orginal article |
Subject:
Other
References
1. Joint WH, World Health Organization. Management of birth defects and haemoglobin disorders: report of a joint WHO-March of Dimes meeting, Geneva, Switzerland, 17-19 May 2006. [URL]
2. Forci K, Bouaiti EA, Alami MH, Mdaghri Alaoui A, Thimou Izgua A. Incidence of neural tube defects and their risk factors within a cohort of Moroccan newborn infants. BMC Pediatrics 2021;21(1):1-0. [DOI:10.1186/s12887-021-02584-5] [PMID] []
3. Rai SK, Singh R, Pandey S, Singh K, Shinde N, Rai S, et al. High incidence of neural tube defects in Northern part of India. Asian J Neurosurg 2016;11(4):352-5. [DOI:10.4103/1793-5482.175628] [PMID] []
4. Moody SA, editor. Principles of developmental genetics. Academic Press; 2014 Sep 2. [URL]
5. Singh V, Raina S, Dewan D, Raina S, Dogra V. Epidemiological study of neural tube defects in Jammu division, India. Int J Res Med Sci 2019;7(3):682. [DOI:10.18203/2320-6012.ijrms20190917]
6. Mailaram S, Nalini Y, Ramana Bai PV, Rani S, Lakshmi V. Neural tube defects: A case series. MRIMS J Health Sci 2021;9(1):34. [DOI:10.4103/mjhs.mjhs_21_20]
7. Garg. S, Saxena. A. K, Aneja. P, Saha. S. A study of incidence of neural tube defects and their pattern in a tertiary care hospital of gurugram. Int J Anat Res 2020;8(1.2):727772-82. [DOI:10.16965/ijar.2019.303]
8. Kanchana UT, Choukimath SM, Reddy P, Sherikar S. Congenital Central Nervous System and Associated Systemic Anomalies in Foetal and Perinatal Autopsy-A Retrospective Study. J Clin Diagn Res 2022;16(2). [DOI:10.7860/JCDR/2022/50885.15968]
9. Struksnæs C, Blaas HK, Vogt C. Autopsy findings of central nervous system anomalies in intact fetuses following termination of pregnancy after prenatal ultrasound diagnosis. Pediatr Dev Pathol 2019;22(6):546-57. [DOI:10.1177/1093526619860385] [PMID]
10. Kale-Jain PP, Kanetkar SR, Dhirajkumar BS, Hulwan AB, Borade P, Vohra NV. Study of Congenital Malformations in Fetal and Early neonatal autopsies. Ann Pathol Lab Med 201;4(4):434-41. [DOI:10.21276/APALM.1272]
11. Sivashankara, Naik V, Babu P, Reddy E, Prasad B, Radha B, Myreddy N, et al. Study of various congenital anomalies in fetal and neonatal autopsy. Int J Res Med Sci 2015;3(5):1114-21. [DOI:10.5455/2320-6012.ijrms20150516]
12. Vinutha SP, Narayanappa D, Manjunath GV, Sujatha MS, Sapna Patel MC, Bhat D. The Spectrum of Congenital Central Nervous System Anomalies Among Stillborn: An Autopsy Based Study. Annf Neurosci 2020;27(3-4):224-31. [DOI:10.1177/0972753121990169] [PMID] []
13. Panduranga C, Kangle R, Suranagi VV, Pilli GS, Patil PV. Anencephaly: A pathological study of 41 cases. J Sci Soc 2012;39:81-4. [DOI:10.4103/0974-5009.101852]
14. Kant S, Malhotra S, Singh AK, Haldar P, Kaur R, Misra P, Gupta N. Prevalence of neural tube defects in a rural area of north india from 2001 to 2014: A population‐based survey. Birth Defec Res 2017;109(3):203-10. [DOI:10.1002/bdra.23578] [PMID]
15. Cherian A, Seena S, Bullock RK, Antony AC. 2005. Incidence of neural tube defects in the least-developed area of India: a population-based study. Lancet 366:930-931. [DOI:10.1016/S0140-6736(05)67319-9] [PMID]
16. Zaganjor I, Sekkarie A, Tsang BL, et al. 2016. Describing the prevalence of neural tube defects worldwide: a systematic literature review. PLoS One 11:e0151586. [DOI:10.1371/journal.pone.0151586] [PMID] []
17. Kulkarni ML, Mathew MA, Reddy V. The range of neural tube defects in southern India. Arch Dis Childh 1989; 64:201-04. [DOI:10.1136/adc.64.2.201] [PMID] []
18. Mini S, Neera A, Shashi V, Bhargava SK. Neural tube defects in an East Delhi Hospital. India Jf Pediatr 1991; 58:363-65. [DOI:10.1007/BF02754968] [PMID]
19. Bhide P, Sagoo GS, Moorthie S, et al. 2013. Systematic review of birth prevalence of neural tube defects in India. Birth Defects Res A Clin Mol Teratol 97:437-43. [DOI:10.1002/bdra.23153] [PMID]
20. Avagliano L, Massa V, George TM, Qureshy S, Bulfamante GP, Finnell RH. Overview on neural tube defects: From development to physical characteristics. Birth Defects Res 2019;111(19):1455-67. [DOI:10.1002/bdr2.1380] [PMID] []
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







 gmail.com
gmail.com