BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijrabms.umsu.ac.ir/article-1-340-en.html

 , Bharathi Sree M
, Bharathi Sree M 

 , Anupama Vubbara
, Anupama Vubbara 
 , Sai Chandana Gali *
, Sai Chandana Gali * 
 , Indrani Gattamneni
, Indrani Gattamneni 

Introduction
Tuberculosis (TB) remains a significant global health burden, with extrapulmonary tuberculosis (EPTB) representing a substantial proportion of cases (1). Tuberculous lymphadenitis, the most common form of EPTB, poses a diagnostic challenge due to its nonspecific clinical presentation (1).
Extrapulmonary tuberculosis (EPTB) refers to clinically diagnosed cases of tuberculosis involving organs other than the lungs, such as the pleura, lymph nodes, abdomen, genitourinary tract, skin, joints, bones, and meninges (2).
Tuberculous lymphadenitis (or tuberculous adenitis) is a form of tuberculosis infection affecting the lymph nodes, leading to lymphadenopathy (3). When cervical lymph nodes are affected, it is commonly referred to as "scrofula" (4). Although the cervical region is most commonly affected, tuberculous lymphadenitis can occur throughout the body, including the axillary and inguinal regions (5).
The stages of tubercular lymphadenitis are as follows (6): I. Lymphadenitis II. Periadenitis III. Cold abscess IV. 'Collar stud' abscess V. Sinus
The major immune responses of the host to tuberculous infection include macrophage activation, specific T-cell-mediated reactivity, and granuloma formation. The tuberculous granuloma is classically described as having a necrotic center surrounded by concentric areas of epithelioid cells, Langhans giant cells, lymphocytes, plasma cells, and fibroblasts (6).
Fine needle aspiration cytology (FNAC) is a valuable diagnostic tool for evaluating lymph node pathology. However, the traditional method of detecting acid-fast bacilli (AFB) using Ziehl-Neelsen (ZN) staining often suffers from low sensitivity, hindering the diagnosis of tuberculous lymphadenitis (4, 5). To address this limitation, this study aimed to evaluate the efficacy of a modified bleach concentration method in improving AFB detection compared to conventional ZN staining.
Liquefaction of lymph node aspirate by sodium hypochlorite (NaOCl, bleach) and concentration of bacilli through centrifugation can significantly increase the sensitivity of direct microscopy (7-9).
This study compared the diagnostic performance of the modified bleach method to the gold standard, the cartridge-based nucleic acid amplification test (CBNAAT). The findings of this study are expected to contribute to improved diagnostic accuracy, early case detection, and effective management of tuberculous lymphadenitis.
Materials and Methods
Study Design:
This was a cross-sectional observational study conducted at the Cytology Department of Pathology, Sri Venkateswara Ramnarayan Ruia Government General Hospital, Tirupati, Andhra Pradesh from October 2023 to March 2024 (6 months) after approval from the Institutional Scientific and Ethics Committee.
Study Population: A total of 146 patients with suspected TB lymphadenitis were included in the study based on the following inclusion and exclusion criteria.
Inclusion Criteria:
1. Patients with clinically suspected TB lymphadenitis referred for FNAC to the Division of Cytopathology in the Department of Pathology.
2. Patients willing to provide written informed consent for the FNAC procedure and participation in the study.
Exclusion Criteria:
1. Patients who had received TB treatment within the previous 3 months.
2. Patients with lymph node swellings suspicious for malignancy.
Methodology: Patients with lymphadenopathy underwent a brief clinical examination. Data regarding age, sex, duration, and description of swelling (including site, number, and size) were documented for each patient.
After explaining the procedure, informed written consent was obtained from each patient. FNA was performed under strict aseptic conditions. The patient was positioned comfortably to expose the target area for aspiration. The type of aspirated material was observed and assessed. Part of the aspirate was sent for CBNAAT analysis at SVRRGGH, Tirupati.
The collected material was processed for cytological examination using direct and alcohol-fixed smears stained with H&E stain. Prepared smears were examined for cytomorphological diagnosis under microscopy. Direct smear microscopy for the detection of AFB was performed immediately after the FNA specimen was collected using conventional ZN staining (Figure 1).
 |
Fig. 1. Conventional ZN Staining procedure for AFB detection
Part of the aspirate was processed using the modified bleach concentration method (Fig. 2). The lymph node aspirate sample was mixed with 2 ml of 5% sodium hypochlorite (NaOCl) in a 5 ml sterile test tube containing 1 ml of normal saline. The mixture was incubated at room temperature for 15 min, with shaking at regular intervals for bleach digestion. After adding 2 ml of distilled water, the test tube containing the mixture was centrifuged at 3000 rpm for 15 min. The supernatant was discarded, and sediments were transferred with a sterile pipette onto a sterile slide for smear preparation. After air-drying, the slide was stained using the conventional ZN staining method.
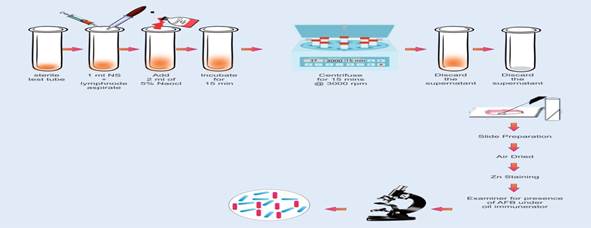 |
Fig. 2. Modified bleach technique procedure for AFB detection
Smears prepared by the conventional ZN staining method and the modified bleach method were examined for AFB under oil immersion (100x) alongside a positive control stained with conventional ZN stain. AFB Grading was performed according to RNTCP guidelines (Table 1).
Table 1. RNTCP guidelines for grading of Tuberculous bacilli
|
Number of bacilli / field |
Result |
Grading |
|
No AFB / 100 fields |
Negative |
|
|
1-9 AFB / 100 fields |
Positive |
Scanty |
|
10-99 AFB / 100 fields |
Positive |
1+ |
|
1 - 10 AFB / field |
Positive |
2+ |
|
>10 AFB / field |
Positive |
3+ |
Cytomorphological diagnosis was compared with results from the ZN method and the Modified bleach method. Both the ZN method and the Modified bleach method were compared with the CBNAAT assay, which served as the gold standard technique.
Data Analysis: Data were analyzed using Microsoft Excel. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated to assess the diagnostic performance of the modified bleach method compared to CBNAAT and the conventional ZN method.
Results
In the present study, 146 cases of clinically suspected tuberculous lymphadenitis were included. The age range of participants was 1 to 85 years, with a mean age of 31 years. Of the 146 cases, the majority were females (87 cases, 59.6%) compared to males (59 cases, 40.4%).
Fine needle aspiration cytology (FNAC) was performed on lymph nodes from various sites: 132 cases (90.4%) from cervical lymph nodes, 6 cases (4.1%) from axillary lymph nodes, 7 cases (4.8%) from inguinal lymph nodes, and 1 case (0.7%) of generalized lymphadenopathy.
Cytomorphological analysis of the 146 cases revealed:
· Reactive lymphadenitis features in 52.05% (76/146) of cases
· Granulomatous lymphadenitis in 43.15% (63/146) of cases
· Suppurative lymphadenitis in 4.79% (7/146) of cases
Using the conventional Ziehl-Neelsen (ZN) method, 44 cases (30.1%) showed acid-fast bacilli. Of these positive cases:
· 5 cases were diagnosed as suppurative lymphadenitis
· 39 cases were diagnosed as granulomatous lymphadenitis (Table 2)
In the conventional Ziehl-Neelsen method, bacteria were identified as pink-colored, slender, rod-shaped, and sometimes beaded or curved bacilli (Fig. 3). Most of the bacilli were observed singly. Slides were graded for positive bacilli according to the RNTCP guidelines for grading Tuberculous bacilli, as shown in Table 1.
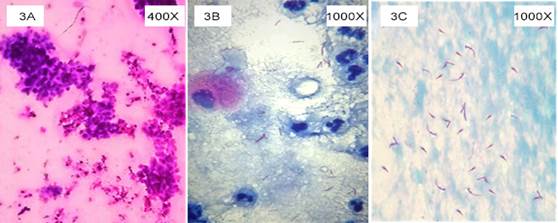
Fig. 3. Microphotograph of suppurative lymphadenitis. 3A- Cytomorphology showing abundant degenerative neutrophils with macrophages against necrotic background. 3B – Smear showing positive (2+) for AFB by conventional ZN method. 3C –Smear showing positive (3+) for AFB by modified bleach method
By modified bleach concentration method 49 cases showed acid fast bacilli. Out of which 5 cases were diagnosed as suppurative lymphadenitis and 44 cases were diagnosed as granulomatous lymphadenitis (Table 2). In comparison with conventional ZN staining method 5 cases showed positive for AFB (Figure 4), which were negative in conventional method (Table 3).
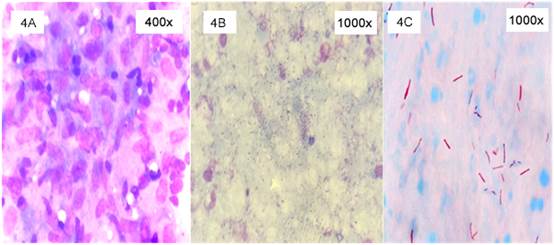
Fig. 4. Microphotograph of granulomatous lymphadenitis. 4A- Cytomorphology showing granuloma with epithelioid macrophages admixed lymphocytes. 4B – Smear showing negative for AFB by conventional ZN method. 4C – Smear showing positive (3+) for AFB by modified bleach method.
By CBNAAT assay, 48 cases were positive for TB bacilli, among 146 cases studied. 4 cases which showed positive for AFB on the conventional ZN method were negative on CBNAAT. 8 cases came out positive for CBNAAT, which were negative for AFB on the conventional ZN staining method (Table 4). Comparison between the conventional Zn method and CBNAAT as the gold standard, showed a sensitivity of 83%, specificity of 96%, positive predictive value (PPV) of 91% negative predictive value (NPV) of 92% (Table 5) similar comparison between modified bleach concentration method and CBNAAT was done, which showed a sensitivity of 98%, specificity of 98%, positive predictive value (PPV) 96% negative predictive value (NPV) 99%.
Table 2. Comparison of cytomorphological diagnosis of ZN method & Modified bleach concentration method
|
Cytological Pattern |
Conventional ZN |
Modified Bleach Method |
Total |
||
|
(+ve) |
(-ve) |
(+ve) |
(-ve) |
||
|
Reactive Lymphadenitis |
0 |
76 |
0 |
76 |
76 |
|
Suppurative Lymphadenitis |
05 |
02 |
05 |
02 |
07 |
|
Granulomatous Lymphadenitis |
39 |
24 |
44 |
19 |
63 |
|
Total Cases |
44 |
102 |
49 |
97 |
146 |
Table 3. Comparison of Conventional ZN method with Modified Bleach concentration method for detection of AFB
|
Zn Method |
Modified bleach method |
Total |
|
|
Positive |
Negative |
|
|
|
Positive |
44 |
0 |
44 |
|
Negative |
05 |
97 |
102 |
|
Total |
49 |
97 |
146 |
Table 4. Comparison of ZN method and Modified Bleach method with CBNAAT
|
Zn Method |
CBNAAT |
Total |
|
|
Positive |
Negative |
|
|
|
Positive |
40 |
4 |
44 |
|
Negative |
8 |
94 |
102 |
|
Total |
48 |
98 |
146 |
|
Modified Bleach Method |
CBNAAT |
Total |
|
|
Positive |
Negative |
|
|
|
Positive |
47 |
2 |
49 |
|
Negative |
01 |
96 |
97 |
|
Total |
48 |
98 |
146 |
Table 5. Statistical comparison between ZN method & Modified Bleach method with CBNAAT
|
|
ZN Method |
Modified bleach method |
|
Sensitivity |
83% |
98% |
|
Specificity |
96% |
98% |
|
Positive Predictive value |
91% |
96% |
|
Negative Predictive value |
92% |
99% |
Discussion
Tuberculosis (TB) remains a major global health concern, being the world's second leading cause of death from a single infectious agent, after coronavirus disease (COVID-19), and causing almost twice as many deaths as HIV/AIDS. TB is caused by the bacillus Mycobacterium tuberculosis (Mtb), which is spread via airborne droplets. Approximately one in four people worldwide demonstrate an immunological response to Mtb infection, which can remain dormant or progress into active disease forms (1). The global public health threat posed by TB necessitates rapid and precise diagnostic tools to enable early treatment initiation and prevent disease spread (10). Thus, there is a critical need for access to fast and accurate detection tests, as well as rapid and accurate drug-susceptibility testing (DST) for all TB patients (11).
Direct microscopy is a fast and inexpensive method to identify acid-fast bacilli (AFB), the majority of which are mycobacteria (12). Traditionally, the Ziehl–Neelsen (ZN) stain has been applied, and samples are termed "smear positive" or "smear negative", depending on the presence or absence of AFB (10). However, the routine ZN stain has low sensitivity. Methods used to increase the sensitivity of the ZN method include the use of NaOCl (bleach), an effective disinfectant that gives a higher density of bacilli per microscopic field, thereby decreasing the AFB detection time of slides.
In the present study, the modified bleach technique demonstrated higher sensitivity (98%) compared to the conventional ZN method (83%). Notably, 5 cases that were negative on the conventional ZN method showed positive results for AFB using the modified bleach technique, which was subsequently confirmed by the CBNAAT assay. This improvement can be explained by changes in the surface properties of the bacilli (i.e., charge and hydrophobicity) and denaturation of the specimen, leading to flocculation and subsequently increased sedimentation rate of the AFB, allowing deposition of bacilli at the bottom of the test tube after centrifugation (13). This method is advantageous in TB control programs where bleach (NaOCl) is affordable and available (13).
Several studies have reported similar findings, demonstrating the improved efficacy of the bleach concentration method over the conventional ZN method. Mandal et al. conducted a study on 63 clinically suspected tubercular lymphadenitis cases, showing an increase in AFB positivity from 36.50% using the conventional ZN method to 61.90% with the bleach concentration method (14). Singh et al. reported an improvement from 40.00% to 63.47% (9), while Chandrasekhar et al. observed a substantial increase from 12.50% to 60.05% (12). However, it's worth noting that not all studies have shown consistent results. Gayathri Purushothaman et al. reported a decrease in AFB detection rate from 30.00% with the conventional method to 20.00% with the modified bleach method (8). In our present study, we observed a modest improvement, with AFB positivity increasing from 30.13% using the conventional ZN method to 33.56% with the bleach concentration method.
The improved sensitivity of the modified bleach method can be attributed to the concentration of AFB during the process, leading to a higher likelihood of detecting even low numbers of bacilli. This has significant implications for the diagnosis and management of tuberculous lymphadenitis, as early and accurate diagnosis is crucial for initiating appropriate treatment and preventing disease progression.
Conclusion
The modified bleach concentration method demonstrated superior performance compared to the conventional ZN staining in detecting AFB in patients with suspected tuberculous lymphadenitis. This study highlights the potential of the modified bleach method as a valuable diagnostic tool for improving the accuracy and efficiency of tuberculosis diagnosis. However, further studies with larger sample sizes and diverse patient populations are warranted to confirm these findings and assess the cost-effectiveness of this method. Implementation of this technique could potentially lead to earlier detection and treatment of tuberculous lymphadenitis, ultimately contributing to better patient outcomes and more effective TB control programs.
Acknowledgements
Nil
Ethical statement
This study was approved by the Institutional Ethics Committee of Sri Venkateshwara Medical College, Tirupati, dated 07/09/2023, with letter number 159/2023. The Institutional Ethics Committee ensured that all ethical principles were adhered to, and the rights of all participants were fully protected.
Data availability
Data will be available as per request.
Author Contributions
Nil
Conflict of interest
There are no conflicts of interest.
Funding
Nil
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




 gmail.com
gmail.com